Save the Brain: Study suggests new way to treat head trauma
When a loved one has suffered a serious head injury, perhaps in a car crash or a fall, relatives and friends hope for the best. But physicians know a sobering truth: There’s little they can do, and the patient stands a good chance of dying or having permanent brain damage.
New observations of how mouse brains react to severe trauma, however, suggest a surprising way to treat head injuries. The rodent data indicate that physicians should consider drugs that do the exact opposite of certain medications that have previously been tested, without success, on people with serious head injuries.
“This is really important and is going to shake the field up a little bit,” says Mary Ellen Michel of the National Institute of Neurological Disorders and Stroke in Rockville, Md.
In a head injury, brain-cell death and damage occur immediately at the impact site. However, in the hours after the injury, many more brain cells elsewhere succumb as initially damaged cells release fluid and neurotransmitters, such as glutamate.
Previous work with rodents and other animals led scientists to theorize that the postinjury flood of glutamate contributes to the delayed cell death by overstimulating nerve cells. So, researchers have given drugs that block those cells’ glutamate receptors to people in the hours and days after a traumatic brain injury.
“All of them failed miserably,” says Anat Biegon of Brookhaven National Laboratory in Upton, N.Y. She and her colleagues in California, Montana, and Israel now propose an explanation. They contend that understimulation of glutamate receptors is the more serious problem in head injuries.
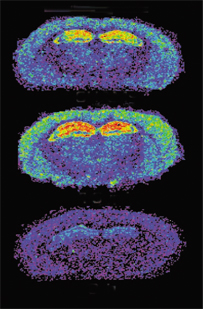
Using a radioactively labeled compound that binds to the active form of the primary glutamate receptor, the investigators analyzed brains slices from mice at different times after each had received a traumatic blow to the head. As expected, an initial burst of receptor activity appeared in the minutes after the injury, presumably from glutamate released by directly damaged cells. In the following hours, however, the activity of this glutamate receptor declined to below-normal levels, Biegon’s team reports in the April 6 Proceedings of the National Academy of Sciences.
In a follow-up experiment, the scientists inflicted head injuries on other mice and then, 24 and 48 hours after the injury, injected some of these rodents with a compound that stimulates the glutamate receptor and others with an inactive solution. When evaluated 1 and 2 weeks later, the mice receiving the compound had recovered more neurological function than the others had.
The scientists “have shown improved functional recovery [in the mice],” says Kenneth I. Strauss, director of the University of Cincinnati’s Mayfield Neurotrauma Research Lab. “They’ve really proved their case well.”
Before considering the use of drugs that stimulate glutamate receptors for people with brain injuries, scientists should examine whether the treatment saves brain cells in mice and whether the animals retain their recovered neurological skills, adds Strauss.
Nonetheless, says Michel, the new study suggests that a relatively late treatment of a head injury could improve a patient’s outcome.







