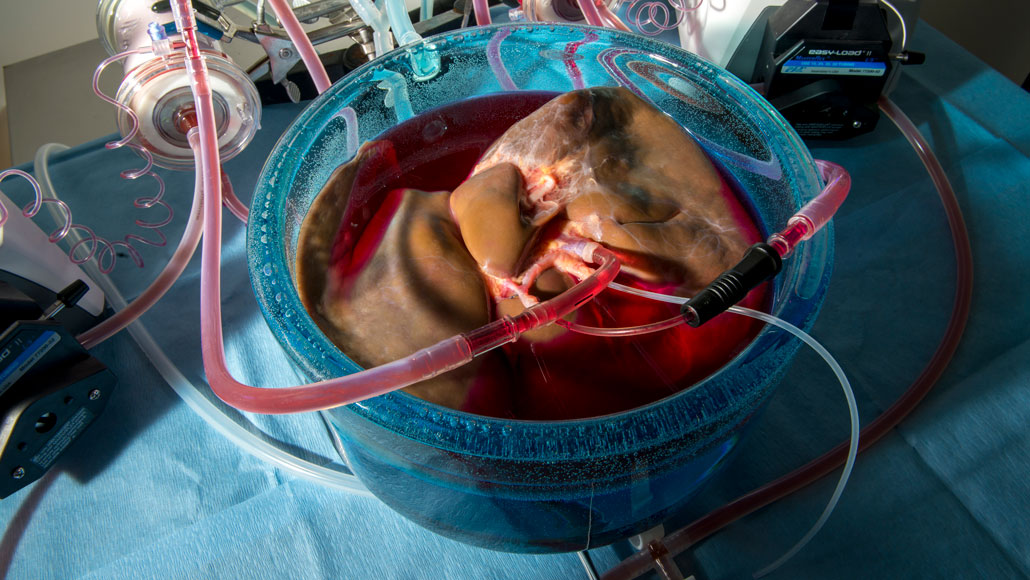
Treating human livers with protective chemicals (red liquid) before storing them at subzero temperatures kept the organs viable for over a full day outside the body — about three times as long as a liver’s normal preservation time on ice.
Jeffrey Andree, Reinier de Vries and Korkut Uygun
A new technique to keep donor organs colder than ice cold could greatly extend the length of time that those organs are viable for transplant.
Typically, donor organs stay viable for several hours on ice at about 4° Celsius. Tissue can last even longer at lower temperatures — but below zero degrees Celsius, the formation of ice crystals risks damaging an organ and rendering it unusable. Now, using chemicals that prevent an organ from freezing at subzero temperatures, researchers have preserved five human livers at –4° C. That supercool storage system tripled the livers’ typical shelf life from nine to 27 hours, researchers report online September 9 in Nature Biotechnology.
This kind of deep-chill technology “would be huge for transplantation,” says Jedediah Lewis, president and CEO of the Organ Preservation Alliance in Berkeley, Calif., a nonprofit that supports research on organ and tissue preservation but was not involved in this research.
Every year, thousands of donor organs are discarded for various reasons, including the inability to find a suitable patient close enough to receive the organ before it goes bad. If donor tissue were viable longer, doctors could get organs to patients who might otherwise be too far away, Lewis says. That could lead to more lifesaving surgeries for patients waiting for a transplant — currently more than 100,000 in the United States alone. Pushing back organs’ expiration dates could also curb the costs of private flights to rush organs between cities and allow for more flexible surgery scheduling, Lewis adds.
In the new study, researchers devised a cocktail of cryoprotectant chemicals, including trehalose and glycerol, to combat ice formation and protect cells at extremely low temperatures. To ensure each liver was completely saturated with preservatives, the researchers administered the chemicals using a machine perfusion system. That device is basically “an artificial body for the liver” that pumps fluids into an organ in a way that imitates blood flow, says Reinier de Vries, a medical doctor and mechanical engineer at Harvard Medical School and Massachusetts General Hospital in Boston.
Demand versus supply
Over the past few decades, the need for organs has skyrocketed while the number of available organs (yellow) has grown very slowly, allowing only a fraction of patients who need a transplant to get one (blue). Supercooling donor organs to extend their viability could increase the number of organs available to patients on the waiting list (brown).
U.S. organ donors, transplants and transplant waiting list, 1991–2018
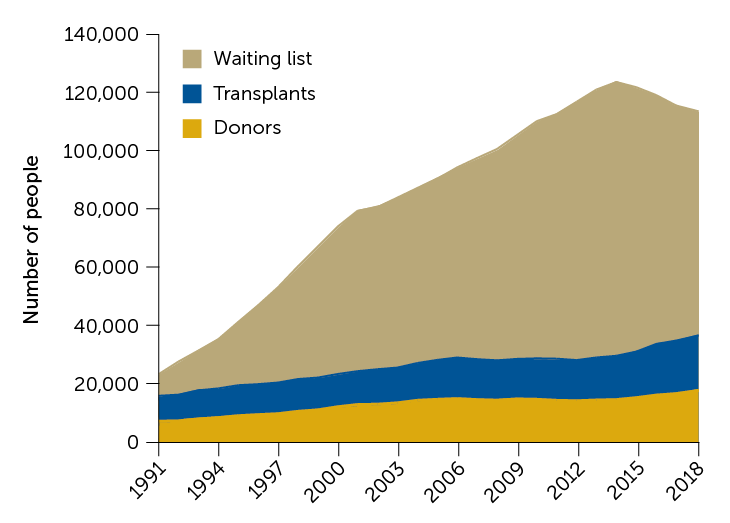
Source: Organdonor.gov
This supercooling preparation scheme is a more sophisticated version of a chemical injection previously shown to preserve rat livers for several days at –6° C (SN: 7/3/14). Additional cryoprotectant chemicals and the more elaborate machine perfusion equipment allowed the new setup to handle human livers, which are harder to supercool because they’re about 200 times as big as their rat counterparts.
Once each human liver was loaded up with cryoprotectants, de Vries and colleagues sealed it in a bag to stash in a chiller at –4° C. After 20 hours in the icebox, the researchers hooked the liver up to a machine perfusion system that flushed out the chemicals that helped it withstand the cold and warmed the organ to room temperature. From start to finish, the supercool storage process took about 27 hours.
In experiments with five livers, “we got absolutely no ice formation for the duration of storage,” says study coauthor Shannon Tessier, a biomedical engineer also at Harvard and Mass General. When the researchers checked the livers for tissue damage and compared how well the livers took up oxygen, produced bile and performed other functions before and after supercooling, the team found no major changes in the organs’ health. Tessier and colleagues then warmed three of these organs to body temperature and infused them with red blood cells and plasma to simulate a transplant, and all remained viable.
To validate the supercool setup, the next step is to transplant organs stored at subzero temps into large animals like pigs, Tessier says. “We actually want to show that the animals survive transplantation,” she says. “Then, hopefully we can think about clinical trials.”
The new supercooling technique “is a really elegant piece of work,” says Malcolm MacConmara, a transplant surgeon at the University of Texas Southwestern Medical Center in Dallas. He imagines that other organs, such as kidneys and hearts, may also benefit from this technology to curb organ shortages (SN: 3/12/19).
Postponing the best-by times for donor organs may be especially useful for organs that deteriorate even faster than the liver, says James Shapiro, a transplant surgeon at the University of Alberta in Edmonton, Canada. “In heart transplants, they like to keep their cold storage times very short — if they go beyond around four hours or so, then the heart surgeons start to get very nervous,” he says. “If you had a system like this that would facilitate longer storage times, you could really open up the possibility of saving more lives.”







