Scientists have added fat cells to the roster of bodily tissues and organs that may harbor infective prions, the renegade misfolded proteins that are believed to cause scrapie in sheep and mad cow disease in cattle. Research on mice infected with scrapie, reported in the Dec. 5 PLoS Pathogens, suggests that fat cells in other animals should also be investigated.
In the new work, scientists examined two strains of mice infected with scrapie, testing tissues including brain, skeletal muscle, tongue, white fat, brown fat, liver and blood plasma for infectivity (meaning that injecting the tissue in a healthy animal would make it sick). Both kinds of fat cells were infective, as were the other tissues, reported a team led by Bruce Chesebro, chief of the National Institutes of Health’s Laboratory of Persistent Viral Diseases in Hamilton, Mont.
Much about prion diseases remains a mystery. The normal version of the protein, called PrP, is found in numerous tissues of humans and many other animals. This protein misfolds in the diseased state, and scientists believe that this nefarious version then coaxes normal PrP to go bad and become toxic. Depending on the strain and host, the result is a disease such as Creutzfeldt-Jakob (CJD) in humans, or chronic wasting disease in elk and deer.
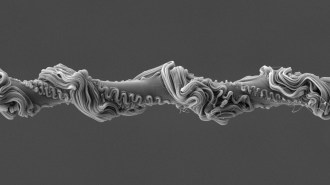
But how this disease-triggering happens isn’t clear. Damage often turns up in nervous system tissues, such as the spinal cord and brain — diseased animals end up with a brain that is pocked with holes. These tissues are also thought to be the most infective. But in the past few years experiments have shown infectivity in multiple organs and tissues in critters from hamsters to sheep to elk.
That fat cells also show infectivity isn’t surprising, says Sina Ghaemmaghami of the Institute for Neurodegenerative Diseases at the University of California, San Francisco. It does highlight the need for diagnostic tests to determine if animals or people are sick. In some versions, the disease can sit silent for years with no external symptoms.
The work also highlights how little is known about prion diseases in general. “It is kind of confusing,” says Chesebro. The prion protein can misfold in more than one way, so more than one version of prion disease can occur in a given animal. The bad proteins are thought to travel via nerves — but researchers are also looking into blood. In humans there is a genetic version of a prion disease linked to a mutation on the PrP gene. Humans also can be affected by the version known as variant CJD, which is linked to eating infected beef — but no one knows how the prions move from the stomach to the brain.
“Unlike any other disease it can be infective, genetic and sporadic,” says Ghaemmaghami. “That is unique to this disease.”