Attention, shoppers: The latest blue light special could help combat diabetes and some genetic diseases.

Scientists have harnessed a light-gathering protein usually found in the eye to turn on the production of a protein that controls blood sugar. Researchers in Switzerland and France rigged kidney cells to make the blood-sugar control protein when exposed to blue light and then implanted diabetic mice with tiny capsules containing the engineered cells. Shining a blue light directly on the mice’s skin or through an implanted optical fiber brought blood sugar levels back to normal, the team reports in the June 24 Science.
Other researchers have switched nerve cells on and off with light-activated proteins (SN: 1/30/10, p. 18), but this is the first time such a system has tackled a metabolic disease in a mammal, says Edward Boyden, a neuroengineer at MIT who was not involved with the study. “They offered a compelling clinical demonstration that you can change the physiological state of an organism,” he says. “It leads to some powerful thinking about what this could lead to.”
The new technique could be used to spur the manufacture of proteins lacking in patients with rare genetic diseases such as phenylketonuria, in which an inability to make an enzyme can lead to brain damage. Modified versions of the system might also help scientists figure out which biochemical processes are going haywire in a wide variety of diseases, Boyden speculates.
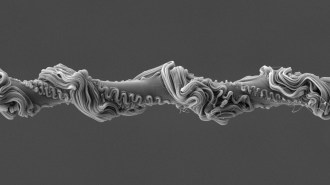
Conceptually, the system is simple. Researchers start with human embryonic kidney cells engineered to make a protein called melanopsin and then insert a gene for whatever other protein they want to produce into the cells. Melanopsin is a light-harvesting protein normally found in the retina of the eye. It responds to blue light and sets off a biochemical chain reaction that sends nerve signals to the brain. Instead of sending nerve signals, the scientists harnessed a chain reaction already present in kidney cells to turn on the inserted gene.
In the new study, shining a blue light on the melanopsin-carrying kidney cells turns on production of a protein called glucagon-like peptide-1, or GLP-1. That protein, in turn, governs production of insulin and other proteins that help control blood sugar levels.
“From the ground up we designed this to be all human,” says study leader Martin Fussenegger, a bioengineer and synthetic biologist at the Swiss Federal Institute of Technology Zurich, located in Basel. Using human cells that make human proteins helps reduce the risk that the immune system would attack the proteins if the technique is ever developed to treat people.
Fussenegger wouldn’t speculate on how long it might be before light-activated cells are treating people with diabetes or other diseases, but says “it’s the first step in a new direction for treatment.”
Engineers may have a few kinks to work out first, though. Bright sunlight or light sources that contain blue wavelengths might activate the system when it’s not wanted. Covering implants with a patch might solve such a dilemma, says Fussenegger. “We’ve never done the experiments at the beach,” he says, but normal indoor lights did not turn on unwanted protein production in the lab.