Here’s what we’ve learned in six months of COVID-19 — and what we still don’t know
Scientists across the globe are racing to crack the mysteries of the novel coronavirus

Over the past six months, the coronavirus pandemic has upended daily life. In most places, social distancing guidelines have become the new normal. For instance, newly reopened restaurants are taking measures to keep customers apart — like this one in Hudson, N.Y.,with plastic barriers between its tables.
Angus Mordant/Bloomberg via Getty Images
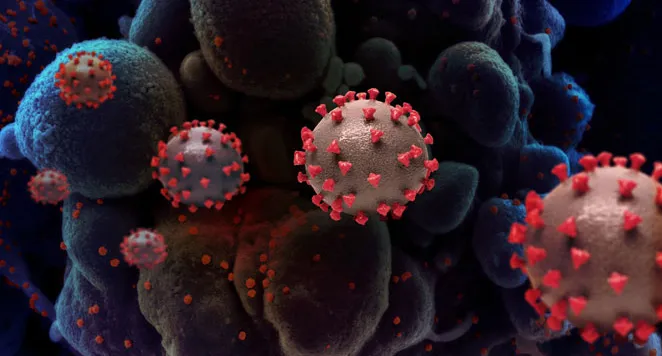
Just six months ago, the World Health Organization got a troubling report from Chinese health officials. A mystery pneumonia had sickened dozens of people in Wuhan. That virus, which had crossed from an unknown animal host to humans, has now upended lives worldwide with head-spinning speed.
Although virologists had long warned of the pandemic potential of some coronaviruses circulating in bats in China, the virus launched a shock-and-awe attack that researchers and public health workers are still scrambling to understand and control (SN: 11/30/17). That attack has upset everything from day-to-day life to entire economies, and turned the routine — going to school, popping into a restaurant, hanging out with friends — risky. The world today is a far different place than when the first reports of an odd pneumonia in Wuhan, China, made the news.
COVID-19:
The first six months
This story is one in a series looking at the first six months of the pandemic.
Now countries have begun to reopen, with fingers crossed that they have a handle on the virus, called SARS-CoV-2. Many are quickly learning that they can’t let down their guard. Officials in Beijing, for instance, reinstated a limited lockdown June 13 in the area around Xinfandi market in response to a cluster of COVID-19 cases. And after New Zealand eradicated the virus and lifted restrictions on June 8, officials confirmed two new cases on June 15 in infected travelers from the United Kingdom.
Other countries never got their outbreaks under enough control in the first place. For instance, while the increase in COVID-19 cases in parts of the United States has ebbed, the number of infections in other places largely spared in the spring, including Texas, Florida and Arizona, is now spiking.
With unprecedented efforts to study the virus and its impacts, scientists have learned an extraordinary amount in an extraordinarily short period of time and overturned some early assumptions. In the beginning, public health officials made recommendations on how the virus might behave and how best to protect oneself from it based on past experiences with two of the pathogen’s close relatives — severe acute respiratory syndrome coronavirus, or SARS-CoV, and Middle Eastern respiratory syndrome coronavirus, or MERS-CoV. But some of those initial assumptions turned out to be wrong, and there’s still much that researchers need to figure out.
What a difference six months makes
Here is a look at how scientists’ understanding of the virus has evolved in the six months since its discovery.
Then
In the first days of the pandemic, Chinese officials reported that the new coronavirus doesn’t easily transmit from person to person.
Now
By January 20, it became clear that the virus can be passed from one human to another, even before symptoms appear, unlike SARS and MERS. People who never display symptoms can also pass the new virus to others.
Then
Coronaviruses like SARS and MERS tend to infect deep in the lungs, so the new coronavirus is probably spread mainly by people with symptoms, such as a cough, or during such medical procedures as being intubated.
Now
In addition to lung cells, SARS-CoV-2 can also infect cells in the nose, which may explain how people can transmit it to others before feeling sick. Talking or breathing may be enough to spread the virus.
Then
The earliest signs of illness include fever, shortness of breath or cough, the U.S. Centers for Disease Control and Prevention listed in January.
Now
A wider range of symptoms, including fatigue, diarrhea and body aches, can suggest a person has COVID-19. One of the clearest signs may be loss of smell and taste.
Then
Older people above age 65 are at highest risk for developing severe disease.
Now
Age is still a risk factor for severe symptoms, but underlying conditions like high blood pressure, obesity and diabetes also boost risk. Racial disparities have also come to light. In the United States, Black, Indigenous and Hispanic people are getting infected or dying at higher rates than white people.
Then
Children are largely spared from the disease.
Now
This is still true relative to other age groups, though researchers aren’t sure why. But low risk doesn’t mean no risk. Some children can develop a dangerous inflammatory condition linked to COVID-19.
Then
An infected person will transmit the virus to two or three other people, on average.
Now
With social distancing and contact tracing, many places, including China, South Korea and New Zealand, have brought the infection rate from two to three down to below one. But in certain regions, including India, Latin America and parts of the United States, people may still be passing the virus on to more than one other person. And without stringent public health measures in place, large gatherings have led to clusters of infections.
Then
Of people who test positive for the virus, around 4 percent die.
Now
Death rates vary due to in part to differences in testing among countries. (For example, if only people with severe disease get tested that might inflate the case fatality rate.) Pinpointing a global rate won’t be clear until the end of the pandemic. But antibody testing has allowed scientists to estimate that the infection fatality rate — a measure that includes people who were not tested, perhaps because they had mild or no symptoms — may be around 0.6 percent in some places.
Then
Only sick people should wear masks, according to guidance from WHO and the CDC.
Now
With data showing asymptomatic people can spread the virus, both agencies now recommend that all people wear masks in public. The effectiveness of fabric masks was in question early on, but studies now suggest that these masks can help curb transmission of the virus — if most people wear them.
Then
There are no treatments for infected people and no vaccines to curb the virus’ spread.
Now
After a rapid push to test existing drugs against the new coronavirus, some have shown promise, while others fell out of the running. Remdesivir may speed recovery in sick patients. Dexamethasone may reduce the risk of death. The malaria drugs hydroxychloroquine and chloroquine have shown no benefit for infected people. More than 150 coronavirus vaccines are in development, with 20 in clinical trials in people.
So what don’t we know yet?
Six months is an incredibly short time to have learned as much as researchers have about a new virus. But there’s still much to learn. Some questions simply take time to answer.
For example, it’s still unclear why the new virus is so much more contagious than its SARS and MERS relatives — each of which have infected fewer than 10,000 people. It’s also unknown how often asymptomatic people spread the virus (SN: 6/9/20).
Some scientists continue to probe how the virus gets in and out of cells and what types of cells it can infect, from lung cells to those in the intestine. Others are on the hunt for what animal the virus jumped into people from, which can help scientists understand how the virus made the jump and guide policies to monitor those animals for related coronaviruses.
In terms of the disease itself, researchers still don’t know how many virus particles a person must be exposed to in order to get sick, or why some people become severely ill and others don’t. Some patients — even those with milder symptoms — may still have long-term health problems after they recover (SN: 4/27/20). And although people who recover appear to make antibodies that protect against a reinfection with the virus, only time will tell how long that immune protection might last. Answers to these and other questions are crucial to those planning how to safely reopen businesses and schools.
One thing scientists do know is that the coronavirus isn’t going away any time soon, if ever. It will take herd immunity, when at least two-thirds of a population has immunity against the virus either because they have been infected or there is a vaccine, to finally begin to curb the pandemic. Both of those goalposts are still far off for now, though some have said there could be a vaccine by the end of the year. As we head into the next six months, researchers will keep learning new things about the virus as quickly as possible. And so the sprint becomes a marathon.
How we went from a mystery illness to a growing global pandemic in six months

The beginning of the pandemic can seem like a lifetime ago. Here are some key events and discoveries.
December 14–27, 2019
Multiple people who had been exposed to the coronavirus at a Wuhan wet food market, called Huanan Seafood Wholesale Market, are hospitalized with a pneumonia-like disease.
December 31
Chinese officials notify the World Health Organization of a cluster of 41 pneumonia cases of unknown cause.
January 9, 2020
WHO announces the culprit behind the pneumonia cases is a novel coronavirus. Its genetic sequence is released a day later.
January 13
The first known case of infection with the novel coronavirus is reported outside of China, in Thailand.
January 21
The first COVID-19 case is reported in the United States, a Seattle man who had recently returned from Wuhan.
January 22
The first lockdown occurs when China shuts down Wuhan, eventually affecting more than 35 million residents.
January 24
The first COVID-19 cases in Europe (in France) are reported. A Lancet retrospective study traces the first known COVID-19 infection back to December 1.
January 30
WHO declares the outbreak a public health emergency.
February 4
More than 2,500 guests and 1,000 crew members aboard the Diamond Princess cruise ship are quarantined off the coast of Japan.

February 9
The death toll from COVID-19 surpasses that of the 2002–03 SARS outbreak, which killed 774 people.
March 11
WHO declares the outbreak a pandemic.
March 16
The first vaccine trials begin in the United States and China.
April 2
The global number of documented cases passes 1 million.
April 3
To curb the spread of COVID-19, the CDC recommends wearing a covering over the nose and mouth in public.
April 28
The United States hits 1 million reported cases.
April 29
The antiviral remdesivir is the first drug found to block the coronavirus and speed recovery.
May
Countries, including the United States, the United Kingdom and Italy, begin to ease lockdown restrictions.
June 16
The steroid dexamethasone is the first drug found to reduce deaths.
June 19
A record high number of worldwide COVID-19 cases — more than 178,000 — is reported on a single day, prompting WHO director general Tedros Adhanom Ghebreyesus to say the pandemic has entered a “new and dangerous phase.” A week later, the world hit a new daily high: 191,000 new cases.
June 28
Global COVID-19 cases surpass 10 million. More than half a million people around the world have died of the disease.
Tina Hesman Saey contributed to this story.

Trustworthy journalism comes at a price.
Scientists and journalists share a core belief in questioning, observing and verifying to reach the truth. Science News reports on crucial research and discovery across science disciplines. We need your financial support to make it happen – every contribution makes a difference.







