The U.S. largely wasted time bought by COVID-19 lockdowns. Now what?
As states reopen, most don’t have adequate ways yet to test, trace and isolate new cases

A large crowd of young people relax on Fort Lauderdale Beach in Florida on June 28 as cases of COVID-19 reach record highs in the state. South Florida beaches are set to close for the July 4 weekend as part of the state’s effort to slow transmission by reinstating social distancing rules.
mpi04/MediaPunch/IPX
From March to May, much of the United States pressed pause. In the face of a new, highly transmissible coronavirus, widespread lockdowns and social distancing were the only tools available to prevent an overwhelming surge in infections and deaths that threatened to overwhelm healthcare systems.
The strategy largely worked to keep most hospitals functioning. The heavy toll after six months — over 125,000 dead from COVID-19 and more than 2 million Americans infected — almost certainly would have been worse without lockdowns.
But these interrupted months were also supposed to buy time for public health authorities to ready other tools, namely widespread testing and contact tracing, to enable a gradual reopening as we wait for a vaccine (SN: 4/29/20).
Now, many experts worry that the United States has largely squandered the time bought by millions of Americans who stayed home, often at significant personal and financial cost. Despite some progress, especially in testing, most of the country’s local health departments still don’t have the workforce or the infrastructure needed to safely relax social distancing.
Yet most states are forging ahead with reopening anyway. Those that reopened quickly, like Florida and Texas, have already reversed course, reimposing some restrictions in an effort to slow a surge in cases now building across much of the South and West.
Where things stand
Many have worried about a “second wave” of COVID-19, perhaps in the fall. But the truth is that we’re still in the middle of the first wave, even as infections have fallen in many other countries initially hit hard by the virus.
Early hot spots like New York City have cooled off, but that decrease in new cases is offset by a surge in states like Texas, Arizona, California and Florida. The resulting plateau in nationwide cases since May has been ticking upward in recent weeks. On June 26, over 45,000 new cases were reported in the United States, surpassing the previous record set two months earlier.
This increase can’t be blamed solely on more testing. Testing capacity has more than doubled in two months to an average 570,000 tests per day from June 23 to June 29. But the percentage of positive results has gone up in some states, indicating that the virus is in fact spreading. Before its stay-at-home orders were lifted May 15, Arizona’s positive test rate was below 5 percent. Since then, it’s climbed, and averaged above 20 percent since mid-June. On June 26, the U.S. Centers for Disease Control and Prevention released data suggesting that the true number of infections is likely 10 times higher than testing shows. The total number of hospitalizations in Arizona and Texas has risen, too.
“We’re starting to see the epidemiological impact of releasing social distancing measures without necessarily having other control measures in place around the country,” says Crystal Watson, a public health preparedness expert at Johns Hopkins Center for Health Security.
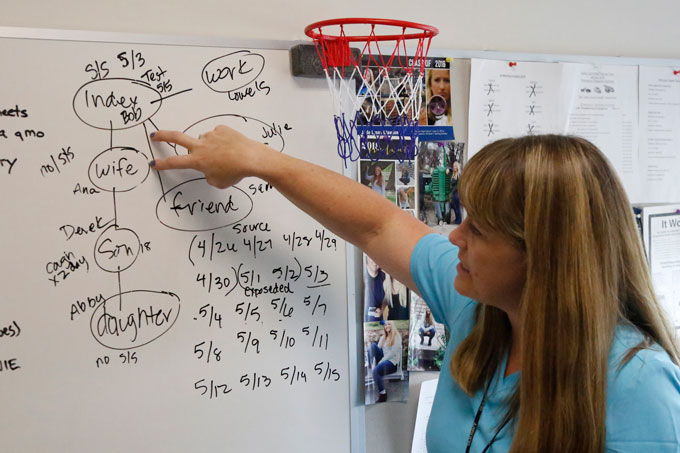
One such measure is contact tracing, which involves local public health officials identifying who a sick person has come in contact with and supporting those who might have been exposed as they self-quarantine to break the transmission chains of the virus (SN: 4/29/20).
But to succeed at tracing, a community must have enough contact tracers to call each new case and investigate that person’s contacts, which takes time and resources. Otherwise, a growing tide of new cases can quickly overwhelm a contact tracing system, leading to an uncontrolled epidemic.
In April, Watson and her colleagues at Johns Hopkins and the Association of State and Territorial Health Officials, or ASTHO, estimated that 100,000 additional contact tracers would need to be trained and deployed nationwide to effectively control the spread of COVID-19 and allow for a safe reopening. “We aren’t close to that number yet,” Watson says.
Currently 37,110 U.S. contact tracers are working on COVID-19, according to a June 18 survey by NPR, which Watson cites as the most up-to-date information. Only seven states and the District of Columbia have a workforce large enough to deal with their current case counts. “Many locations have increased their contact tracing capacity by orders of magnitude in a few months, which is fantastic,” Watson says, “but we still have a long way to go.”
A decentralized, underfunded system
This slow and uneven response stems in part from the decentralized structure of U.S. public health departments. There is no national public health system. Instead, each state, territory or tribal authority runs its own, with varying levels of coordination among counties. “The system has its pros and cons,” says Marcus Plescia, ASTHO’s chief medical officer.
This distributed system allows communities to tailor services to the needs of those they serve, which makes sense since the public health needs of Atlanta, for instance, are very different than those of Lander, Wyo. But it can be difficult to coordinate quick action across the country in response to a threat like COVID-19.
In a more centralized system “there could be opportunities to move faster, but we’re not going to be able to change the system in the middle of a pandemic. We have to work with what we’ve got,” Plescia says.
Local health departments know how to do contact tracing; most have been doing it for diseases like tuberculosis and HIV for years. “But that local infrastructure hasn’t been well funded or prioritized in many communities,” says Candice Chen, a health policy expert at George Washington University in Washington, D.C. Federal funding for public health preparedness has fallen 28 percent since 2005, according to the Johns Hopkins and ASTHO report, and 50,000 workers have been lost since 2008, leaving many small, under-resourced teams largely unable to deal with a crisis as large as the pandemic.
The CDC offers some guidance to local health departments on how to boost contact tracing. And as of late April, states can apply through the CDC for federal funding that’s available through the CARES Act, a federal COVID-19 relief package signed into law March 27. But in the absence of a robust and coordinated federal plan, departments have had to figure out on their own how to boost their contact tracing capacity. Some have managed better than others.
Success story
Anne Arundel County, on Maryland’s Chesapeake Bay, has fared well. In March, early in the pandemic, a team of seven nurses in the county’s epidemiology department was able to handle COVID-19 contact tracing for the county of over 500,000 people, alongside its normal workload, says Jennifer Schneider, the county’s deputy director of disease prevention and management. But when cases kept climbing, “the whole department changed direction,” she says.
Nurses from other programs were diverted to the contact tracing team. Then, when schools closed, the health department reassigned school nurses, who are employees of the county’s health department, to be contact tracers.
“We wouldn’t be able to do what we’re doing now without our school nurses,” whose skills allowed them to quickly pick up the work, Schneider says.
Teams of about eight work in shifts to talk through self-isolation with new positive cases. Then the nurses track down and notify the person’s contacts who’ve potentially been exposed to the virus and instruct them how to quarantine. That can often mean more than just a phone call.
We summarize the week's scientific breakthroughs every Thursday.
“If someone needs food or rental assistance, we’ll work to connect them with the relevant resources,” Schneider says. The department even provides thermometers, following up with cases and contacts each day to ask about their temperature and symptoms.
At peak demand, the county employed 101 contact tracers and was “able to manage the workload well,” Schneider says. So far, Anne Arundel County has seen over 5,000 confirmed COVID cases, but numbers have been falling in recent weeks. Staff diverted to tracing have started resuming their normal work.
With fall fast approaching, department officials are already planning how to expand the contact tracing workforce in the event of another surge, especially if nurses are back in schools. The officials have applied for federal funding to hire more contact tracers to supplement existing staff.
“Anne Arundel County is a case study of strong local health department leadership who knows what they’ve got in their system and can train them for contact tracing,” says Chen.
Unfortunately, such success stories are the exception. Maryland is one of 37 states that don’t have enough contact tracers or reserve staff to meet current caseloads, per NPR’s estimate, much less a future spike. Officials in Bellingham, Wash., for example, are already reporting that a recent surge in cases has exceeded their capacity; cases are falling through the cracks.
Where do we go from here?
No one can know what the next six months will bring, but many epidemiologists are worried that the patchwork system in place won’t be able to contain the virus as communities reopen, especially once fall arrives. While it’s not too late to continue building up contact tracing systems, much damage has already been done.
“We already have major outbreaks going on, and I think the main driver behind this rise is apathy towards the virus,” says Michael Mina, an epidemiologist at Harvard University. “People are sick of social distancing, and understandably so.”
Mina worries that the politicization of the pandemic, and of effective measures like mask-wearing, will further feed the virus’ spread (SN: 6/26/20). “My fear is that come the fall, we’re going to have uncontrolled epidemics that explode and overwhelm health systems.”

Some states, like Oregon and Louisiana, have paused reopening in the face of climbing cases. If ICUs fill up and doctors have to triage healthcare, “places without adequate control systems may have to revert back to something more stringent,” such as shutting some businesses down or reinstating stay-at-home orders, says Natalie Dean, a biostatistician at the University of Florida in Gainesville. Texas, for instance, recently re-shuttered bars and limited restaurant seating capacity.“Nobody wants that, but we may not have a choice, and the lost time that could’ve been used to build up these systems will become really apparent,” she says.
States could also tighten requirements for measures such as social distancing and mask use, which are now voluntary across much of the U.S. patchwork. It’s already mandatory to wear masks in public places in California, New York, Michigan and a growing list of other states.
In light of the spottiness of contact tracing and an inadequate federal response, limiting the spread of COVID-19 in the United States in the months ahead may rest largely on the shoulders of individuals. “We’re waiting around for something to save us, but there’s no silver bullet,” Dean says. “We know things that work; we know how to limit transmission on the individual level.” Wearing masks and practicing social distancing will save lives, as long as people collectively keep up those practices.