The first CRISPR therapy approved in the U.S. will treat sickle cell disease
The gene-editing treatment aims to help people with recurring pain crises
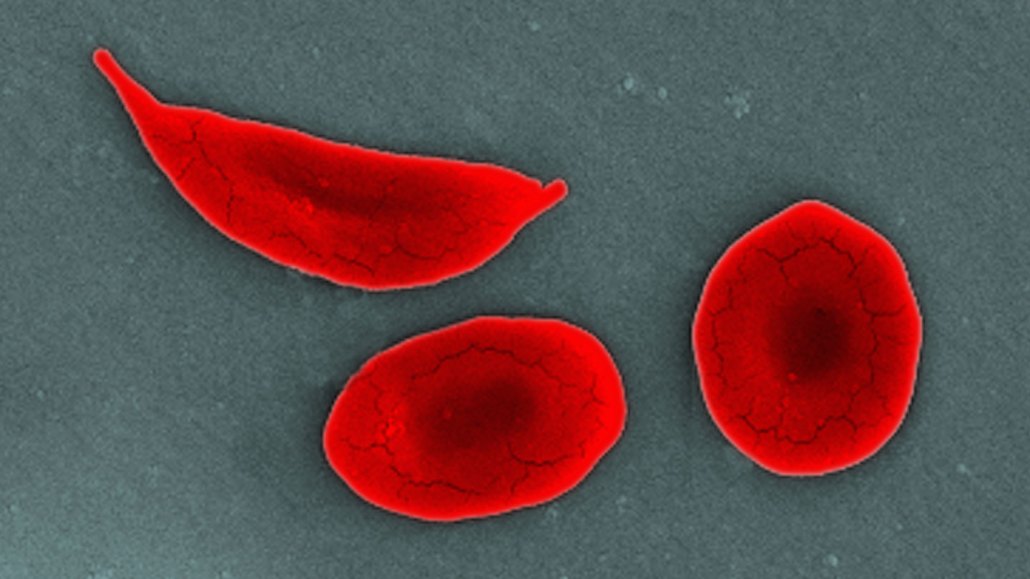
People with sickle cell disease have inflexible, curved blood cells (shown in this SEM image) that get stuck in blood vessels and block blood flow to tissues, causing bouts of debilitating pain.
Callista Images/Getty Images
- More than 2 years ago
U.S. patients with sickle cell disease now have a novel treatment option: the first-ever CRISPR-based therapy.
On December 8, the U.S. Food and Drug Administration approved the gene-editing therapy for use in patients age 12 years and older. In addition to offering hope of relief for people with severe forms of the painful blood disorder, the treatment, called Casgevy, is the world’s first to genetically tweak cells using the Nobel Prize–winning molecular scissors CRISPR/Cas9 (SN: 10/7/20).
Another gene therapy for sickle cell disease, called Lyfgenia and developed by biotech company bluebird bio, based in Somerville, Mass., was also approved December 8.
Getting a green light for the first CRISPR-based medicine is exciting, says David Altshuler, chief scientific officer at Boston-based Vertex Pharmaceuticals, which developed the drug in a joint venture with CRISPR Therapeutics, a company in Cambridge, Mass. But the fact that the drug fills an unmet need for underserved patients is “more compelling to me, personally, than the fact that it’s CRISPR.”
Approximately 100,000 people in the United States, most of them Black or Latino, have sickle cell disease. It is caused by a genetic defect in hemoglobin, the oxygen-carrying protein in red blood cells. Unlike typical blood cells that are bendy enough to slip through blood vessels, sickled blood cells are inflexible and get stuck, restricting blood flow and causing debilitating pain (SN: 2/1/22). People with severe forms of the disease can be hospitalized multiple times a year.
Having a new treatment option for sickle cell disease can give patients a “new lease on life,” says Kerry Morrone, a pediatric hematologist at Albert Einstein College of Medicine in New York City. People with the disease often miss school, work or special events due to excruciating pain. “The potential that this therapy could alleviate symptoms for patients is very exciting.”
At an FDA advisory committee meeting on October 31, several clinical trial participants given Casgevy recounted how it changed their lives, including Victoria Gray, the first sickle cell patient to enroll in the trial.
Gray has previously described bouts of pain that felt like being struck by lightning and getting hit by a train at the same time (SN: 10/20/23). Now pain-free, she is able to enjoy time with her family, Gray said at the meeting.
Jimi Olaghere, another participant in the trial, told a similar tale. Before the treatment, “sickle cell disease dominated every facet of my life,” he said. “Hospital admissions were so regular that they even had a bed reserved for me.” Now, Olaghere is free of pain and able to be present for his children. “Gene therapy has given me the ability to take full control of my life,” he said. “I can chase to the proverbial sunset and write novels and even dance in the rain without a care in the world.”
There are few existing therapies for sickle cell disease, which include taking drugs like hydroxyurea or undergoing bone marrow transplants (SN: 12/17/20). But hydroxyurea doesn’t work for everyone, and transplants require a genetically matched donor, usually a sibling. Less than 20 percent of people with sickle cell disease have a matched sibling.
Casgevy is like a transplant, but instead relies on a patient’s own cells. Using CRISPR, the treatment alters the genetic blueprint of bone marrow cells that give rise to blood cells. The edited cells make fetal hemoglobin, a type normally made by fetuses and young babies that doesn’t make red blood cells sickle and gum up vessels (SN: 8/14/19).
Patients first receive chemotherapy to wipe out existing bone marrow cells so the new ones, which are edited in a lab, have a chance to thrive in the body. After editing, the cells are given back to the patient through an IV. Both steps require hospitalization.
In a clinical trial, 29 out of 30 patients given Casgevy and followed for at least 16 months didn’t have pain crises for at least a year, Vertex vice president of clinical development William Hobbs said at the FDA advisory committee meeting.
The treatment isn’t without risks. Chemotherapy, for instance, can raise the risk of blood cancer and cause infertility. And in the short-term, chemotherapy kills immune cells, putting patients at higher risk dying from infections.
For some patients those risks may pale in comparison to the prospect of a year without immense pain, says Morrone, who is also director of the Sickle Cell Program at the Children’s Hospital at Montefiore. Others may want to wait and see what the outcomes are. “I think that’s fair, because it’s not without any risk.”
At the Oct. 31 meeting, advisors to the FDA also discussed the potential for unintended edits, or “off-target effects.” An analysis by Vertex found no evidence of such unwanted changes in treated patients, although researchers have identified a rare variation in the DNA of some people that could, in theory, be an accidental target.
It’s unknown whether changing that accidental target would have consequences for patients, but researchers say it’s unlikely because that stretch of DNA isn’t involved in a protein’s structure or function. Nor is the protein made from that genetic code found in blood cells. Overall, the 14-member committee agreed that the benefits of the treatment were clear and the off-target risk is small, but that additional research would be helpful.
Another concern is that the therapy is expensive, perhaps as much as $2 million per patient. But health care costs for sickle cell patients are also high over their lifetime, Morrone says. The health care community needs to consider ways to ensure equity for patients — including in Africa, where the highest burden of disease is — who have long not had the same resources as patients with other conditions with far more treatment options. “There’s not a value on suffering,” she says.
On November 16, officials in the United Kingdom became the first to sign off on Casgevy’s use in sickle cell patients as well as people with beta-thalassemia, a blood disorder in which the body doesn’t make enough hemoglobin. The FDA will decide by March 30 whether the CRISPR therapy can also be used to treat beta-thalassemia by March 30.
Senior staff writer Tina Hesman Saey contributed to this story.







